Practice management
Psychiatry/patient selection
Pediatric consent
- <18yo have to have consent from at least one parent (unless emancipated)
- Alternatives to a procedure are a part of informed consent, nature of surgery, diagnosis, indications, benefits, consequences, side effects, risks, consequences of alternatives, probability of success
- Minors should not be put at risk due to parents religious beliefs, “bloodless” surgery still provides physician with emergency transfusion if life depends on it
- emancipation – marriage, military service, financial independence, living apart from parents, parenthood
- legally able to consent for medical procedures
BDD
- preoccupation with perceived flaws that seem minor/slight to most others
- repetitive behavior or mental acts related to appearance concerns
- preoccupation causes significant distress and impaired daily function
- Eating disorders may be seen but are not critical to diagnosis
- BDD is most commonly associated with depression (75%)
- Psychological contraindications to surgery: when success is dependent on goals (job promotion marriage etc), must be seen frequently post-operatively
Statistics
statistical power
- a measure of the number of subjects in comparison to the effect size, test size, and power of the test
- can determine a sample size or verify a nonsignificant result after data collection.
- ideal power = 80%
P value
- the probability that the result happened by chance
- a low P value (usually <0.05) means that there’s a less than 5% chance that the observed results happened due to chance/sampling variation. so you can feel confident rejecting the null hypothesis.
Types of tests
- categorical variables –> pearsons chi-squared test
- numeric variables –> regression analysis
- independent numerical, dependent categorical –> ANOVA
- nonparametric tests – wilcoxon rank-sum, kruskal-wallis test
- Numerical and dependent categorical variables: unpaired T tests and ANOVA
Errors
- Type I: you think theres an effect when there really isnt (rejecting the null hypothesis when it is true)
- Protect by setting a higher alpha
- Type II: you think theres no effect but actually there is
- Increase your power
- Type III: rejecting the null hypothesis for the wrong reason
- Type IV: incorrect interpretation of a correctly rejected hypothesis
Levels of studies
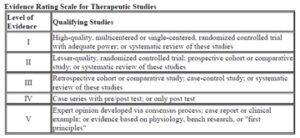
- I – high quality blinded RCT with adequate power, or systematic review of these
- II – lower quality RCT, prospective cohort, or systematic review of these
- III – retrospective cohort study, case-control study, or systematic review of these
- IV – case series
- V – expert opinion consensus, case report, or evidence based on physiology principles/bench research
Specificity – the ability of a test to correctly classify an individual as disease free (ratio of those classified as disease free and total number of healthy patients)
d/b+d
Sensitivity – the ability of a test to correctly classify an individual as diseased
a/a+c
Ratio of those classified as having the disease over the total number of sick patients
Legislature
Charity –
- participating in charity cannot imply or provide a financial incentive to have a procedure
- does not imply understanding of a performance or procedure for which the patient has not been medically evaluated yet
- injectables like botox are appropriate
- no procedures, no implants
Certificate of need – to coordinate planning of new services while controlling costs for production/building
Advertising board eligible while still seeking initial certification – only ok for 8 years
- after that, boards every 10 years
EHR
- computerized provider order entry is the preferred method for entering orders, otherwise a written or verbal with readback
- CMS EHR Enrollment gives you 1% penalty adjustments below existing medicare/medicaid reimbursements for failure to participate in the meaningful use of certified EH technology on a yearly basis
- Meaningful use of EMR = increasing the ability of health care systems to protect patient medical information in compliance with HIPAA regulations- using the approved EMR systems to their full potential in order to provide optimization of health care data documentation to improve the quality of health care
- using the approved EMR systems to their full potential in order to optimize documentation to improve the quality of care delivered
- improve quality/safety/efficacy/reduce disparities
- engage patients and families
- improve care coordination
- improve population/public health
- ensure privacy/security protection for PHI
Universal protocol for preventing wrong site, wrong procedure and wrong person surgery
- preop patient identification by three members of the team
- preoperative marking of the surgical site
- final time-out prior to surgery or procedure
Government in Sunshine act – open payments – CMS publishes med devices/pharmaceutical rep payments of over a certain amount to physicians
ADA – requires that reasonable accommodations are provided by businesses and in public areas to allow people with disabilities to participate in daily activities
- HIPAA (health insurance portability and accountability act): rights including restricting information, inspecting records, amending records, can audit disclosure of records (covers health plans, clearinghouses, and providers)
- Can waive IRB/HIPAA if preparing research protocol or performing research on someone who has died
- IRB approval must have deidentified information-strip records of any identifying information or have statistician approve small contribution to identification
- Requires standardization of electronic health care
- Disclosures: per request of patient, for treatment or payment, to individuals identified by patient, incidental disclosure, limited data set with removal of identifiers, public interest groups
- PHI
- name, address, birth date, SSN
- past/present/future physical or mental health condition
- provision of health care to the individual
- payment for the provision of health care to the individual
- For payment, must sign HIPAA wavers in matters of dispute , cannot send documentation without signed consent
- PHI can only be shared between two treating healthcare professionals in a confidential/encrypted communication not at risk of breach or theft
- To store patient photos on computer must be encrypted using an approved process
- privacy official is a responsibly body for privacy in an organization – can range from an individual who functions as the privacy official at a small practice, to a full time position
- Ambulatory surgery requirements: AAASF, must be board certified (with any board), general anesthesia requires 12-24 hours of oversight, must have unrestricted privileges within 30 minutes , pediatric patients need to be PALS trained by one member, inspected q3 years
- “new patient” – hasn’t been seen in the same specialty in the same practice in 3yr
- Use of a medical assistant does not increase medico-legal risk, witness is not part of the integral consent process
- Cannot use ASPS logo until board certified
- Office based procedures: need appropriate drugs, resuscitation, and intubation equipment, defibrillator
- Disciplinary action: charging exorbitant fees (especially in emergencies), charity events in which surgery is performed, endorsement compensations, false pictures- not typical results or photographic techniques that misrepresent
- Potential hires: do not ask about disabilities, age, arrests, children, religion, country of origin, race, child care
- If not treating patient, must obtain verbal consent to view and share information
- When you prescribe medication to friend, friend becomes patient and must document this encounter
Errors
- near miss – unplanned event that does not result in injury/illness/damage but has the potential to do so
- look-alike sound-alike medication error – giving or prescribing wrong medication because it looks or sounds similar
Health insurance
Billing
- physician bills for an amount.
- insurance decides how much the service is worth, and that is how much the physician will get. (the difference is not considered debt or anything)
- the actual payment may come partially from the insurance company and partially from the patient, depending on their “co-pay” agreement.
Medicare
- A – hospitalizations, SNF, hospice (usually included if you are over 65 or if you are under 65 but collect social security benefits)
- B – provider and related services ie doctors, PT, labs, equipment, mental health
- C – additional approved private health insurance
- D – prescription drug coverage
- Medicare payments: difference of bill and payment is considered contractural adjustment and services are paid in full (physician agrees to accept payment according to medicare fee schedule)- payment from medicare and copayment
ACA – must offer 10 essential health benefits
- outpatient care, ER visits, hospitalization, maternity/newborn, mental health/substance use treatments, prescription drugs, rehab + equipment, lab tests, preventative services and chronic disease care, pediatric services including dental and vision.
- does not cover adult dental or vision
- Insurance companies do not cover elective cosmetic procedures, patient must be billed separately; must inform OR when switching to cosmetic portion of procedure
ACGME
Core competencies
- interpersonal and communication skills
- medical knowledge
- patient care and procedural skills
- professionalism
- systems based practice (ACGME milestone)
- coordinating patient care within health systems, cost awareness, patient advocacy, interprofessional development
Miscellaneous
- Cameras: for optimal reproducible digital photographs and pre- and post op need matching anatomical landmarks, same camera/lens/lighting/patient position
- Grid pattern, 2 lenses, single lens with 50-60mm marco, 90-105 focal for facial, 2 light sources, sky blue uncluttered background
Source:
ACAPS Inservice exam questions 2015-2020